Pain Assessment Tool Form offers the guidelines for patient’s evaluation. Health care professionals use this handy tool to determine pain intensity, location, and interference along with temporal pattern. This form offers a platform for determining the course of the treatment and helps in preventing exacerbating.
However, trained professionals like nurses must evaluate the patient’s pain using this assessment tool. This pain assessment tool offers scopes to record the findings graphically as well as in scales. Please complete all fields duly for accurate evaluation of pain and the recurrence pattern. You may choose to use this tool on intermittent frequencies for regular review of pain.
These regular reviews of pain using this assessment tool help in determining the response to the treatment. Please keep all these forms safely in the patient’s case history file for record. Pain Assessment Tool Form simplifies pain management by defining each essential element.
How To Prepare Pain Assessment Tool Form
- Enter patients name on the first line of the assessment tool form. Then mention admission reference number. Please enter the date of running the evaluation using this form.
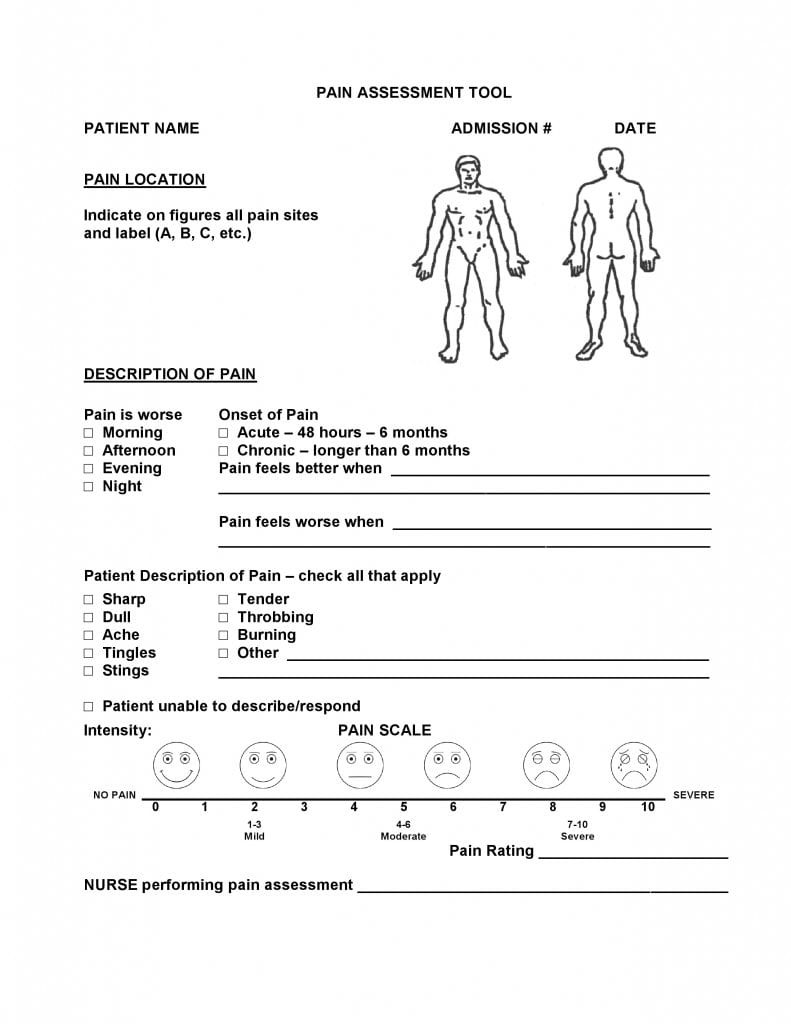
- Please mark pain sites on the figures provided in the form. You may choose to label each site as directed. Use any ink other than black to mark these painful sites on the figures.
- Please describe the pain as directed in the form. Select the right option if the pain is worse in the morning, afternoon, evening or night by marking the correct box before each option. You may select more than one box in this category.
- Describe onset of pain by marking the box to select acute (within 48 hours – 6 months) or chronic (longer than six months).
- Describe when the patient feels better and when the pain worsens by confirming the same from the patient. Please be very specific while filling information as pain is subjective symptom.
- Ask the patient to describe the pain. You may select the appropriate option to describe the pain from the available choices like Sharp, Dull, Ache, Tingles, Sting, Tender, Throbbing, Burning, and any other type. Please specify descriptively in case you select option Other.
- Mark the next box in case the patient is not in a position to respond to your questions or describe the pain accurately.
- Next graphic representation helps in determining the scale of pain intensity. Please follow pain rating as directed. (1 to 3 for mild pain, 4 to 6 for moderate pain, and 7 to 10 for severe pain. Specify your rating for patient’s pain on the next line.
- The nurse performing this assessment using the Pain Assessment Tool Form must endorse the test by entering his/her name, employee ID, and signature.
Form Preview